At every stage of human development and maturation, vitamin A profoundly impacts the formation and training of both tissue-resident and humoral immune cells. Vitamin A insufficiency occurs on a global scale, and even in developed nations, poor eating habits can reduce intakes of vitamin A and its precursors while inflammatory, atopic, and infectious conditions heighten the body’s need for them.
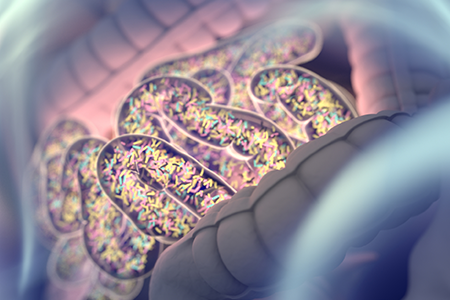
Recent research clarifies that vitamin A is not just an immune activator, inhibitor, or adjuvant. On the contrary, vitamin A metabolites engage in constant interaction with other immune factors and cytokines—especially in the gut—to help customize an ideal immune response and then facilitate immune tolerance.
This review details clinical and pre-clinical evidence of how the vitamin A metabolite retinoic acid (RA) cooperates with local immune responses, and even more importantly, helps coordinate these efforts with intestinal immunosurveillance in order to optimize the whole-body response to immune challenges. They describe mechanisms linking immunity at crucial epithelial borders (such as the skin, gut, and respiratory surfaces) with other humoral and cellular immune actions as well as the formation of immune memory and tolerance.
Vitamin A Status Minds Gut Mucosal Immunity

KEY TAKEAWAY:
Vitamin A as RA shows a broad capacity for favoring immune tolerance while facilitating an effective acute immune response. These actions are particularly efficient as the result of vitamin A’s targeting of gut-related immune cells and lymphoid tissues. However, nutritional sufficiency of vitamin A and its precursors at all stages of life is necessary for this healthful range of immunomodulation. Vitamin A insufficiency results in the opposite, enabling chronic immune dysregulation and inflammation to occur.